If you think of your immune system as a city, T cells are the skilled responders, the detectives, firefighters, and paramedics who rush in when trouble appears. They identify threats like viruses or cancer cells, coordinate the rest of the immune force and when needed, take out the bad guys directly. But as with any busy city, you also need traffic cops to keep things from turning chaotic. That’s where regulatory T cells, or Tregs, come in. They don’t chase criminals; they prevent pileups – calming responses so your body doesn’t harm itself.
What makes a T cell a T cell?
Every T cell carries a special sensor on its surface called a T-cell receptor (TCR). Think of it as a lock designed to fit one very specific key. The “key” is a tiny piece of a peptide surface marker displayed to T cells by other cells in your body, called the major histocompatibility complex (MHC). There are two main types for T cells:
CD8 T cells read peptides on MHC class I, which most cells carry. These are the hit-team cells: if they see a virus-infected or cancerous cell, they can destroy it.
CD4 T cells read peptides on MHC class II, found on professional sentry cells (like dendritic cells). CD4s are the coordinators, shaping how the wider immune response unfolds.
T cells don’t act on a whim. They usually need three green lights: a match between their receptor and the peptide, a “costimulation” handshake confirming the danger is real, and a set of cytokines (immune signals) that tell them which role to take on.
T cell boot camp
Before they get their badge, T cells go to school in a small organ above the heart called the thymus. Here, immature T cells are tested. If can they recognize the body’s MHC they are selected. If they do not recognize the body very well (a red flag for autoimmunity) they are removed. Graduates leave as naïve T cells – experienced enough to patrol, but not yet assigned to a specific job.
The T cell career ladder
Once a naïve T cell meets its matching “key” during an infection, or cancer, it specializes.
Effector T cells are short-term doers. They multiply quickly and either kill infected cells or coordinate other immune cells.
Memory T cells are long-term guardians. They stick around after the battle so next time, the response is faster and stronger. You’ll find them as central memory (lives in lymph nodes), effector memory (circulates in blood and tissues), and tissue-resident memory (parks in places like the skin or lungs).
The main T cell teams
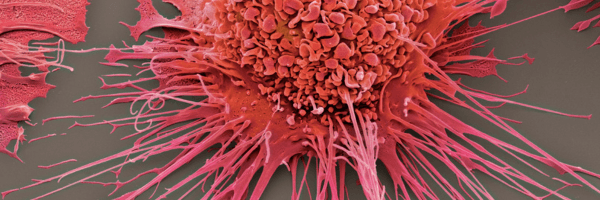
CD8 “cytotoxic” T cells are the direct fighters. When they recognize an infected or abnormal cell, they can trigger it to self-destruct using protein “grenades” called perforin and granzymes. When CD8 cells recognize a target (virus-infected or tumor), they release perforin to punch transient pores in the target membrane, then deliver granzymes inside to trigger programmed cell death. They also release interferon-gamma, a signal that boosts the body’s ability to control viruses and cancer.
CD4 “coach” T cells have the same badge, different job. CD4s set strategy by differentiating into different subtypes, called T-Helper (Th) cells:
- Th1 cells push a strong anti-virus, anti-bacteria response and activate “big eaters” called macrophages.
- Th2 cells recruit eosinophils and mast cells – important for parasites and, yes, also involved in allergies.
- Th17 cells help defend our body’s borders (skin, gut) and tackle fungi and certain bacteria.
- Tfh (follicular helper) cells are the B-cell whisperers, helping B cells make better, longer-lasting antibodies.
These labels aren’t rigid. T cells adapt as situations change, which is part of what makes them so powerful, and sometimes, if misdirected, harmful.
Meet the peacemakers, the Regulatory T cells (Tregs)
Tregs are a special subset of CD4 T cells. Their job is not to fight, but to prevent friendly fire. They carry a hallmark protein called FOXP3 and often a high amount of CD25, a receptor that soaks up growth signals other T cells need. You can think of Tregs as the immune system’s brakes.
Some Tregs are born that way in the thymus. They tend to recognize self-signals and are essential for preventing autoimmunity. Others are made out in the body when regular CD4 T cells are exposed to calm-down signals like TGF-β and IL-2. These are peripheral or induced Tregs, often found at barrier tissues like the gut where you need a light touch.
How do Tregs calm things down?
Tregs release soothing cytokines like IL-10 and TGF-β that reduce inflammation. They soak up IL-2, a growth factor, making it harder for over-excited T cells to multiply out of control. They use CTLA-4, a surface brake that dials down the “costimulation” on sentry cells, so fewer T cells get revved up. In some settings, they can directly silence or even kill overactive immune cells, or change the metabolism of nearby cells to a calmer state.
When Tregs don’t work, the city goes haywire: people with rare mutations in FOXP3 develop severe autoimmune disease early in life. On the flip side, some tumors recruit extra Tregs to keep anti-cancer T cells quiet – an immune shield for the cancer.
Checkpoint brakes and accelerators
T cells wear both gas pedals and brakes on their surface. CD28 and friends are accelerators, while CTLA-4 and PD-1 are brakes known as checkpoints. Cancer immunotherapy often works by blocking the brakes (with “checkpoint inhibitor” drugs that target PD-1 or CTLA-4), letting fighter T cells do more. This can be life-saving, but also increases the risk of immune side effects, which makes sense: you’re lifting the brakes.
What this means for real life
Infections: A healthy T-cell team clears viruses and bacteria, then powers down. Tregs help end the fight cleanly so you don’t suffer unnecessary collateral damage.
Autoimmunity: If T cells aim at the wrong target, or if Tregs are too few or too weak, the immune system can attack your own tissues (think type 1 diabetes, multiple sclerosis, rheumatoid arthritis).
Cancer: You want strong, focused T-cell fighters. But if the tumor recruits Tregs or flips on lots of checkpoints, it can hide in plain sight. That’s why some cancer treatments try to block checkpoints or reduce Treg influence inside tumors
Transplantation & allergies: Tregs are heroes here. Boosting Treg function can promote tolerance, accepting a transplanted organ or calming allergic inflammation.
Testing your immune system with the Lymphocyte Map test
We use the Lymphocyte MAP test from Cyrex labs to take a “headcount and balance check” of your white-blood-cell teams, the T cells, B cells, and natural killer (NK) cells and a few T-helper sub-teams (like Th1, Th2, Th17, and T-regs). It tells us “Is your immune system balanced or leaning one way?” For example, more “allergy-type” activity (Th2), more “inflammation/autoimmune-type” activity (Th1/Th17), or not enough brakes (T-regs).
We get back a report with bars/percentages for each cell group and a simple summary “immunotype,” e.g., “balanced,” “Th2-skewed,” or “low NK activity,” plus key ratios. This gives us a snapshot of immune tone when dealing with things like autoimmunity, frequent infections, allergies/asthma, chronic inflammation, or to track response to lifestyle/therapies that aim to calm or rebalance immunity.
How we use results (examples):
- High Th2 / low Th1: fits with allergy-leaning patterns → focus on allergy control, gut/airway triggers, sleep, stress; sometimes guides which therapies to try
- High Th17 / low T-reg: suggests inflammatory/autoimmune tilt → reinforces anti-inflammatory strategies and closer medical follow-up
- Low NK cells: may help explain frequent viral infections and prompt further work-up of nutrients, sleep, meds, etc
- CD4/CD8 ratio off: can reflect immune activation or suppression and may prompt targeted follow-up
Keep your immune system healthy
There’s no superfood that “creates T cells,” but basic health habits help your immune system run smoothly. Sleep is when your immune system updates its playbook. Movement supports circulation and stress balance, which helps immune surveillance. Vaccination trains memory T cells without the danger of full-blown disease. Stress management matters; chronic stress can dysregulate immune responses. Nutrition supplies the building blocks immune cells need; extremes (starvation, ultraprocessed overload) don’t help.
T cells are your immune system’s precision team. CD8s take out infected or cancerous cell, while CD4s coordinate strategy and boost antibody responses. Over the top of all this, Tregs keep everything balanced ensuring your defenders don’t turn into wrecking crews. When the fighters and the brakes are in the right proportion, your immune “city” thrives.
Author
Scott Rollins, MD, is Board Certified with the American Board of Family Practice and the American Board of Anti-Aging and Regenerative Medicine. He specializes in bioidentical hormone replacement for men and women, thyroid and adrenal disorders, fibromyalgia and other complex medical conditions. He is founder and medical director of the Integrative Medicine Center of Western Colorado (www.imcwc.com) and Bellezza Laser Aesthetics (www.bellezzalaser.com). Call (970) 245-6911 for an appointment or more information.