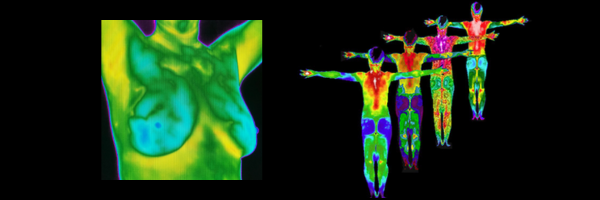
Breast thermography is a quick, painless, no contact imaging technique that can be part of an early detection program for breast cancer. Using no radiation, thermography picks up heat using an infra-red imaging system. Physiologic changes such as infection, inflammation or increases in blood flow are often the source of abnormal heat patterns that may encourage cancer or be present during very early stages of cancer.
The diagnostic quality when screening for breast cancer has improved to a level where it is comparable to mammography, particularly given the limited sensitivity of mammography in young women and those with dense breast tissue. Thermography may be performed years before standard mammograms are ordered thus allowing increased screening.
Also, they pick up functional changes that may predate the development of cancer thus providing an opportunity to prevent cancer development in the first place. This gives patients an opportunity at targeted behaviors that can truly lower the chance of developing cancer, such as improving their diet, exercising more, or stopping smoking. Of course these are things we should all be doing anyway, but sometimes screening tests are motivation for change. Also, conditions such as estrogen dominance may be suggested by a thermogram and this is a more subtle situation that a functional medicine doctor may need to help with.
If certain abnormalities are found on a thermogram it may trigger additional studies, such as a mammogram or ultrasound, thus thermograms may be looked at as an adjunct for conventional studies.
The Downside of Mammograms
Mammograms often lead to over diagnosis, over treatment, and don’t substantially reduce the death rate from breast cancer. A 2012 study from the New England Journal of Medicine found that over a 30 year period breast cancer was over diagnosed, meaning that tumors were detected on screening that would never have led to clinical symptoms, in 1.3 million women. They estimated that in 2008 alone, breast cancer was over diagnosed in more than 70,000 women which accounted for about 1/3 of all breast cancers diagnosed.
Meanwhile, in the same study, the number of women presenting with late stage cancers only decreased 8%, leaving the authors to conclude “the imbalance suggests that there is substantial overdiagnosis, accounting for nearly a third of all newly diagnosed breast cancers, and that screening is having, at best, only a small effect on the rate of death from breast cancer.”
Another study, from the Cochrane Database of Systematic Reviews, found very little or no reduction in the incidence of advanced cancers with screening, concluding that “for every 2000 women invited for screening throughout 10 years, one will avoid dying of breast cancer and 10 healthy women, who would not have been diagnosed if there had not been screening, will be treated unnecessarily. Furthermore, more than 200 women will experience important psychological distress including anxiety and uncertainty for years because of false positive findings.”
Exposure to ionizing radiation is yet another concern with mammograms. For many women the procedure is painful. And like many screening tests in medicine, mammograms provide early detection, not prevention.
Scheduling a Thermogram
In collaboration with Aspen Thermography, we offer breast screening thermography once a month at our office. Call our office at 970-245-6911 for details.
Thermography, specifically breast thermography, uses infrared technology to detect heat patterns and blood flow in breast tissues. The TH (Thermographic) ratings, also known as thermographic assessments or thermobiological standards, are classifications used to evaluate the risk of breast abnormalities detected through thermography. These ratings help in assessing the likelihood of underlying pathology, including breast cancer. Here’s a breakdown of what these ratings typically entail:
Thermographic Ratings (TH Ratings)
The TH rating system usually ranges from TH1 to TH5, with each level indicating a different degree of risk:
- TH1 (Normal):
- Description: This rating indicates normal thermal symmetry between both breasts with no significant hot spots or abnormal heat patterns.
- Risk Level: Low or no risk of pathology.
- Recommendation: Routine follow-up and standard screening.
- TH2 (Low Risk):
- Description: Slight asymmetry in heat patterns may be present but within normal physiological variations.
- Risk Level: Low risk of pathology.
- Recommendation: Continued routine follow-up, possibly with a slightly shorter interval than for TH1.
- TH3 (Equivocal/Suspicious):
- Description: Moderate asymmetry or unusual heat patterns that are not typical of normal variations. This may indicate inflammation or benign conditions but warrants further investigation.
- Risk Level: Moderate risk, needs further evaluation.
- Recommendation: Additional diagnostic tests such as mammography, ultrasound, or MRI to rule out malignancy.
- TH4 (Abnormal):
- Description: Significant asymmetry or pronounced hot spots that are highly suggestive of pathological changes, possibly indicating a tumor or other abnormality.
- Risk Level: High risk of pathology, likely requires immediate attention.
- Recommendation: Prompt and comprehensive diagnostic work-up including imaging and possibly biopsy to determine the cause of the abnormal thermographic findings.
- TH5 (Very Abnormal):
- Description: Marked and intense heat patterns, highly asymmetric and consistent with serious pathology such as advanced malignancy.
- Risk Level: Very high risk, likely indicates the presence of cancer or other serious condition.
- Recommendation: Urgent and thorough diagnostic evaluation and referral to a breast specialist for further management.
Additional Considerations
- Symmetry: A key aspect of thermographic assessment is the symmetry of thermal patterns between both breasts. Significant asymmetry often raises concern.
- Vascular Patterns: Unusual or prominent vascular patterns seen in thermograms can indicate increased blood flow typically associated with tumor growth.
- Clinical Correlation: Thermographic findings should always be correlated with clinical examination and patient history for accurate interpretation.
Importance of Follow-Up
Thermography is a screening tool and not a definitive diagnostic method. Abnormal thermographic findings (TH3 and above) should always be followed up with additional diagnostic tests such as:
- Mammography
- Ultrasound
- Magnetic Resonance Imaging (MRI)
- Biopsy, if indicated