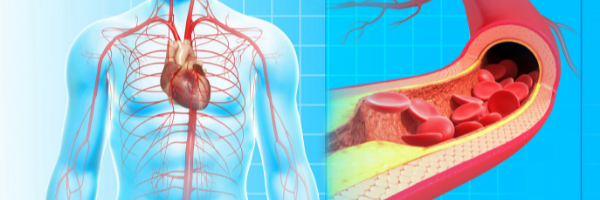
Cholesterol is our friend. It’s part of every cell membrane in the body, a good portion of brain material, precursor to our helpful steroid hormones, and involved in the repair of artery wall defects. But, cholesterol is also what makes up the plaques that clog the arteries to the heart leading to a heart attack, or form small plaques that break loose and float upstream to cause a stroke.
Yet confoundingly, half the people dying from the leading cause of death, that is heart disease, have fairly normal cholesterol. And many people with high cholesterol have clean arteries. How can this be? Because making plaque is NOT ALL about cholesterol.
Plaque Formation
Think of cholesterol and plaque like the woodpile and a fire. You need the woodpile for the fire, but you also need a “spark” and the right conditions for a fire. In a similar manner, cholesterol only leads to plaque under the right circumstances. There are “sparks” that drive cholesterol to make plaque, and certain conditions that favor plaque.
Cholesterol is only bad after it oxidizes. Just like iron rusts, because we live on the oxygen rich planet earth, we oxidize. Only the low density lipoprotein, or LDL cholesterol, oxidizes to start the process of making plaque, first by expressing chemicals that attract white blood cells to the area, which fuels more inflammation and oxidation creating the enlarging plaque.
The second thing oxidized LDL cholesterol causes is the secretion of chemicals that break down tissue. This weakens the artery eventually leading to a rupture of the lining that formed a “cap” over the inflamed plaque. When the plaque ruptures it spills into the artery causing a sudden and complete clotting of the blood, leading to a clogged artery and a heart attack. Or a small plaque may float downstream into the brain and cause a stroke. This is why LDL is called the “bad” cholesterol!
The cells that line the arteries are called “endothelial” cells and they help control cholesterol oxidation as well as blood pressure. But with aging, unlucky genetics, unhealthy lifestyles, poor diet and environmental toxins, especially heavy metals, the endothelial cells take a hit and can’t do their job. Keeping endothelial cells healthy is key to healthy arteries.
There is a misconception that plaque slowly accumulates until it clogs the artery. The coronary arteries which supply blood to the heart muscle need to be 70-80% clogged before the blood flow is restricted enough to cause symptoms such as chest pain. Truth is, most people having a heart attack don’t have even a 50% narrowing before the unstable inflamed plaque ruptures causing a sudden artery clog and heart attack. This is why most people get no warning before their first heart attack. It’s also why someone in apparent good health, could go for a long run one day and keel over dead from a heart attack the next.
Advanced Plaque Detection
How does one know if you have plaque, and if so whether it’s stable or unstable? First, look for it. We tend to make plaque in 3 main places, the carotid arteries, coronary arteries, and the big aorta as it goes through the abdomen to the legs. These are areas of high blood flow, near the heart, with lots of shear damage to delicate endothelial cells.
Screen for plaque with a carotid artery ultrasound. Most hospital and traveling screening ultrasounds only show if you have substantial blockage. A more advanced and sensitive ultrasound can be done which measures the artery thickness, plaque thickness and whether plaque is soft and active, or hard and inactive. It’s the wet juicy soft plaque that kills us. The ultrasound screening I recommend gives a carotid intima-media thickness (CIMT) and is called a CIMT scan.
Another great screening test is a Cardiac Calcium CT scan, which is a three-dimensional x-ray that shows calcium build up in the artery wall. It takes just a few minutes and is available at Community Hospital. Both of these screening tests cost about $200 and are available with a physician’s order. Call our office if you’d like to get screened.
If you screen your arteries, and find absolutely no plaque, then maybe repeat test every 2-3 years to insure things are still ok. If you find any plaque, especially the soft active type, then I recommend more advanced blood tests to analyze why you are making plaque.
Advanced Blood Tests
The basic lipid panel is still a helpful test, including the total cholesterol, low density lipoprotein (LDL), the high density lipoprotein (HDL) and triglycerides (the main fat that is carried in the LDL and HDL packages). As LDL cholesterol is bad, the HDL cholesterol is the “good” cholesterol because if basically offsets all the bad actions of LDL. HDL is protective. The total cholesterol / HDL ratio is actually a good number to watch. Increased LDL is a bad thing, with <100 being really good, and >190 being high enough to meet criteria for medication such as statin drugs. HDL >50-60 is really good.
There are several subtypes of LDL cholesterol though that tell a larger story of risk. One, is an especially bad type of LDL cholesterol called lipoprotein-little-a (Lp-a) which is known as the “heart attack marker” and if elevated puts you at 3x the risk of a heart attack. Second, is the size of the LDL particles, and having small dense (sdLDL) particles that tend to stick and oxidize puts you another 3x the risk of a heart attack.
What makes LDL and HDL what they are, is determined by the type of protein marker in the wall of the cholesterol particle, sort of like a hood ornament on a car. A marker called apolipoprotein A (apoA1) is embedded in each HDL particles, and apolipoprotein B (apoB) embedded in each LDL particle. Inside both particles are pretty much the same thing, a combination of cholesterol and triglyceride fats. It’s the apoA or apoB proteins that determine the cholesterol particle behavior.
Whereas HDL and LDL measurements are the total cholesterol payload, the apoA1 and apoB markers measure the numbers of HDL and LDL particles. Using the car analogy again, one might have the same LDL in one large dumptruck load, or in many small cars, either way totaling the same LDL amount. The best profile is a high apoA1 and a low apoB, and/or a high apoA/apoB ratio.
Example: Someone has an LDL of 90 which is good, but can be deceiving because they could have a high number of LDL particles (apoB) and high % of the small and dense LDL particles (sdLDL) in which case the risk for plaque formation is quite high.
The PLAC test is a blood test used to measure serum activity of lipoprotein-associated phospholipase A2 (LpPLA2), an enzyme that breaks down oxidized LDL in the vascular wall. Higher levels of LpPLA2 activity are thought to promote plaque formation. If the PLAC test is high, this may indicate that the plaque is more likely to rupture.
Markers of inflammation such as high-sensitivity or cardiac-CRP, homocysteine, and omega-6 fatty acids can all give one a warning that the conditions are ripe for plaque formation. Newer tests that predict advancing inflamed plaque such as lipid peroxidase, myeloperoxidase and F2-isoprostanes are just recently available. Measuring the thickness of blood, or blood viscosity is yet another marker that can be used to predict risk of plaque.
Low levels of vitamin D, vitamin K and testosterone are independent risk factors for the formation of artery plaque. I might also check fibrinogen, which measures the tendency of blood to clot. Insulin is yet another marker as high insulin increases plaque risk.
With advanced imaging studies we can determine who has plaque and how active it is. By using more detailed blood testing one can more accurately determine why they are making plaque, better target the cause, and then get busy reversing it starting with lifestyle adjustments, nutritional supplements, and finally medications.
Author
Scott Rollins, MD, is Board Certified with the American Board of Family Practice and the American Board of Anti-Aging and Regenerative Medicine. He specializes in bioidentical hormone replacement for men and women, thyroid and adrenal disorders, fibromyalgia and other complex medical conditions. He is founder and medical director of the Integrative Medicine Center of Western Colorado (www.imcwc.com) and Bellezza Laser Aesthetics (www.bellezzalaser.com). Call (970) 245-6911 for an appointment or more information.